Temboromandibular Joint Disorders (TMJ)
Overview
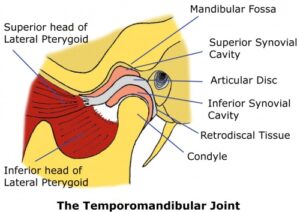
The temporomandibular joint (TMJ) is the hinge that connects the mandible to the skull. There is one TMJ on each side.
TMJ disorders can cause pain in the jaw joint and in the muscles that control jaw movement.
The causes of TMJ disorders can be many. Most of the times, there is no clear-cut cause for the symptoms – idiopathic pain. Previous jaw injury or arthritis can cause TMJ disorders. Clenching or grinding teeth has been linked to TMJ pathology, although the link is questioned.
TMJ disorder is a chronic condition, with episodes of pain and discomfort followed by long asymptomatic or quiescent periods. The condition can be self-managed most of the times, with nonsurgical treatments. Specific interventions and surgery are typically offered in selected cases with promising results.
Symptoms
- Pain on the jaw during eating, speaking or yawning
- Pain over the TMJ and the associated masticatory muscles
- Aching facial pain
- Clicking or locking of the joint, making it difficult to open or close the mouth
- Headaches, aching tension-type pain around the ear and neck
- History of teeth clench or grinding
Causes
The TMJ is a hinge joint that connects the jawbone with the skull. The bony parts are covered with cartilage and are separated by a disk, which allows smooth sliding of the joint. Clearly, any condition that can damage the disc or the joint (trauma, arthritis, disc misalignment) can cause TMJ disorder. However, in the majority of the cases, the cause of TMJ disorder isn’t clear.
Risk factors
- Arthritis (rheumatoid arthritis, osteoarthritis)
- Previous trauma
- Clenching and grinding of the teeth
Examination
Your OMFS Surgeon will check how far you can open your mouth, and record any deviation, pain, clicking or locking during your jaw movements. He will feel your joint and the muscles of mastication for pain and tension. He will examine your occlusion (the way you bite your teeth together) and checks for signs of grinding.
Investigations
Plain X-Rays don’t have a role in TMJ disorders, but they are often used to exclude underlying bony or dental pathology. The gold standard investigation is an MRI scan of your TM joints; it will highlight any disc or soft tissue pathology.
Treatment
Sometimes, the symptoms are so mild that no treatment is needed. The most important step in the management of this condition is the understanding and acceptance by the patient that this is a chronic condition, with often no clear cause and no definitive treatment. It is a condition that is managed rather than treated, and the aim is to make the quiescent periods longer, and the painful periods easier. This understanding makes the patient part of the treatment and is called biofeedback.
Exercises – Jaw Physiotherapy
- Give your joint and muscles rest: Avoid overuse, have soft diet, cut food (i.e. apples) in small pieces and chew slowly for longer, don’t chew gum, don’t bite your nails, support your jaw when yawning. Effective counselling about the condition will be given to you by your OMFS surgeon
- Specific exercises: Like every other painful joint in the body, stretching and massage can help. Your OMFS Surgeon will show you how to do exercises and/or refer you for physiotherapy.
Medications
- Painkillers and anti-inflammatories:Non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen are very helpful in this condition. Topically applied NSAIDs, such as Voltarol cream, can act quickly and reduce the pain.
- Antidepressants:Medications, such as amitriptyline, mostly used for depression, have an analgesic effect and they are often prescribed.
Non-Surgical Therapies
- Mouth guards: Your OMFS surgeon may instruct your dentist to build an appliance that you will wear over your lower teeth (splint or mouth guard). Some patients can benefit from this device, and the philosophy behind its use is the relief of muscle tension around the joint. However, they don’t work for every patient.
Interventions and Surgical Treatments
- Arthrocentesis:This is a minimally invasive procedure that involves the insertion of two needles into the joint so that the joint capsule can be washed and medications (like steroids) can be injected in the joint.
- Botox Injections.Recently, the injection of botulinum toxin type A (Botox,) into the jaw masticatory muscles has shown to alleviate the pain in TMJ disorders. This is a very easy technique; it has minimal drawbacks, and is completely reversible, as Botox action wears off in 3-4 months. The injections can also eliminate headaches resulting from teeth grinding, and, in cases of severe stress they can reduce the incidence of locking.
How does Botox work in TMJ disorders?
Botox reduces the spasm of the masticatory muscles that are attached onto or around the TMJ. “Overworking” or tense muscles can lead to teeth grinding and pain, hence, reducing their action can be beneficial for the symptoms. Most patients experience improvement within one or two days, although full relief can take up to a week. Occasionally, the treatment might not work, if the cause of the TMJ disorder isn’t muscle-related. On these cases, Botox injection can be diagnostic.
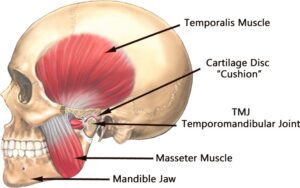
Where will Botox be injected?
Botox is usually injected in the temporalis, masseter and frontalis muscles. Rarely, the pterygoid muscles might be injected, but access is slightly more difficult. The treatment is usually completed within 10-30 minutes.
Risks of Botox Injections for TMJ disorder
As with any procedure there are possible risks and side effects, but these are temporary, minimal and infrequent. The most common reported side effects of Botox treatment are headaches, flu-like syndrome, pain and redness at the injection side, and nausea. Occasionally, there might be bruising on the injection side. Another limitation to Botox injections for TMJ treatments is that there is a possibility of developing antibodies that would render the TMJ treatments less and less effective over time. Botox injection treatments should be avoided during pregnancy and lactation.
- TMJ arthroscopy: Arthroscopy can be both diagnostic and therapeutic. Like any other joint, it facilitates the use of an arthroscope (camera-like instrument), to look and guide instruments. The indications are limited.
- Shaving of the condylar head: This procedure addresses some of the causes of TMJ disorder, by removing part of the bony part of the joint (the head of the mandibular condyle). It can be useful for painful locking cases.
- Eminectomy: This procedure removes the zygomatic eminence that is located in front of the joint. It is indicated for locking or recurrent dislocation problems.
- Open-joint surgery: This is reserved for cases that do not respond to any other treatments and it aims to repair or replace the joint. Occasionally, the disc might be removed (if destroyed) and a fat graft from your abdomen might be placed. Open surgery procedures have risks, and your OMFS surgeon will discuss in detail prior to embark in any of these.
Alternative medicine
Occasionally, alternative therapies have shown benefit in TMJ disorders, but the evidence to support these is limited.
- Relaxation techniques
- Biofeedback
Useful links