Salivary gland diseases
Overview
The salivary glands produce saliva and release it into the mouth. The saliva keeps the mouth moist, protects the teeth from decay, and helps food digestion. There are 3 pairs of major salivary glands:
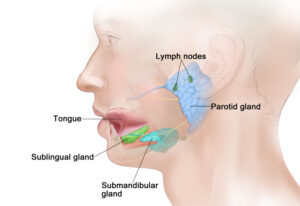
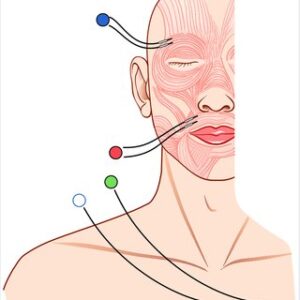
- Parotid glands: These are the largest salivary glands and are found in front of and just below each ear.
- Sublingual glands: These glands are found under the tongue in the floor of the mouth.
- Submandibular glands: These glands are found below the jawbone.
There are also hundreds of small (minor) salivary glands lining parts of the mouth, nose, and larynx.
There are a number of diseases that can affect your salivary glands. These range from cancer to simple infections or autoimmune conditions.
Broadly, salivary gland diseases are categorized in
- Infections
- Tumors
- Cysts
- Sialolithiasis or obstructive diseases (“blocked” salivary glands)
- Autoimmune conditions
Infections
Acute sialadenitis
Acute sialadenitis is an infection involving a salivary gland. Most commonly, it affects the parotid or the submandibular salivary gland. Most unilateral cases of acute sialadenitis are due to bacteria (staphylococcus or streptococcus) and usually there is an underlying predisposing factor (i.e. obstruction of the gland due to stone). Older adults are more likely to develop this condition, especially in the parotid salivary gland (acute bacterial parotitis).

Symptoms include painful swelling in the area of the parotid gland (in front of the ear) or the submandibular salivary gland (under the jaw). There might be pus draining inside the mouth through the salivary gland ducts. The patient might have fever and feel unwell.
Treatment
Initial treatment is rehydration and antibiotics. The patient might require intravenous antibiotics, and intravenous fluids. The patient is encouraged to drink plenty of fluids and lemon juice, to stimulate the saliva production so that the gland is cleared/washed out. Once the acute infection is resolved, the patient will need investigations to identify any underlying causes for obstruction. Once a cause (i.e. stone) is identified, your OMFS surgeon will recommend appropriate treatment.
Acute sialadenitis might also be caused from viruses. Mumps is a well-known cause of bilateral parotitis, but this is now rarely seen due to the success of children vaccination programs. Other viruses that can cause sialadenitis include the flu virus, CMV, EBC, and Coxsackie.

Patients positive for HIV can manifest a rare condition called chronic sclerosing sialadenitis of the submandibular salivary glands: Both submandibular glands appear hard and occasionally painful; differential diagnosis with a tumor is often difficult. This condition is actually called Kutner’s tumor. Once the diagnosis is made, no treatment is needed.
Chronic sialadenitis
This condition is characterized by recurrent episodes of infection in one or more salivary glands. It usually affects the parotid or the submandibular salivary glands. Treatment is usually conservative, with massage and stimulation of saliva production (i.e. with lemon juice). An investigation used to examine for obstruction (sialogram) can also be beneficial from the symptoms point of view, as it washes out any small stones and debris from the ductal system of the gland
Cases that recur very often or when the patient cannot manage the symptoms are suitable for surgery, which involves removal of the salivary gland
Tumors of the salivary glands
Salivary gland tumors can be benign or malignant. Malignant salivary gland tumors are part of the spectrum of Head and Neck Cancer, and they are discussed elsewhere (link to page)
Benign salivary gland tumors are more common than cancer. The parotid salivary gland is the most common side. The most common benign tumor is the pleomorphic adenoma.

It is said that about 70% of parotid salivary gland tumors are benign, and of those, 70% represent pleomorphic adenomas (PSA). This tumor is benign, but it can exhibit malignant transformation if left untreated for many years. It tends to grow and tends to recur if it is not completely excised surgically. The treatment is complete surgical excision, either with a partial superficial parotidectomy, or (in selected cases) with a technique called extracapsular dissection (ECD – excision of the tumor with careful dissection around its “capsule”).
Pleomorphic adenomas can also arise in the submandibular salivary gland and any of the minor salivary glands, but this is more rare.
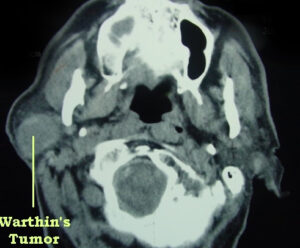
Another benign tumor is the Warthin’s tumor (papillary cystadenoma). This is a cystic tumor that contains lymphocytes and germinal centers. It is believed that it originates from a cystic transformation of a lymph node. Unless it causes symptoms, it doesn’t need treatment. However, excision is often required to confirm the diagnosis. It presents in the parotid gland in the vast majority of cases.
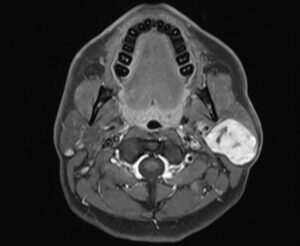
Benign tumors of the salivary gland usually present with a slowly growing painless swelling. Investigations include fine needle aspiration (FNA), to identify the nature of the tumor. An ultrasound scan is a useful first line investigation, as it can provide information on the nature of the tumor and guide the FNA. Finally, an MRI scan will outline the tumor and help planning the surgical treatment.
Cysts
Cysts of the parotid glands present with a swelling and can mimic benign tumors. The diagnosis is easy, as they have a characteristic appearance on the ultrasound, and can be drained to completion via needle aspiration. The cystic fluid has a yellow, straw-like appearance. Unless very large or symptomatic, they don’t need treatment. If the patient wishes, the can be surgically removed.
Mucoceles are pseudocysts that result form injuries to minor salivary glands. They most commonly appear on the lower lip, usually as a result of lip biting. They are filled with mucinous saliva. Treatment consists of surgical removal of the mucocele and the associated minor salivary gland.
A ranula is essentially a mucocele that is formed in the region of the sublingual salivary gland. Occasionally, it can be large and plunging through the floor of the mouth into the neck (plunging ranula). Treatment consists of surgical excision of the ranula and removal of the related sublingual salivary gland.
Sialolithiasis – obstructive disease
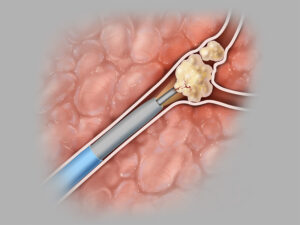
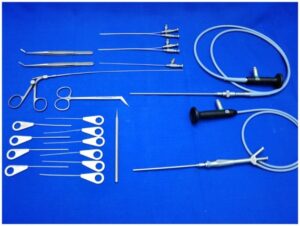
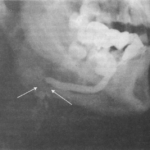
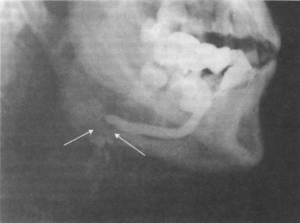
This occurs when stones made of calcium form in the salivary glands. They are more common in the submandibular salivary gland. These stones can block the glands, and can partially or completely stop the flow of saliva. The patients complain of recurrent painful swelling of the gland, which occurs during or immediately after a meal (post-prandial swelling). The stone is often obvious in an occlusal dental X-ray, and your OMFS surgeon might be able to feel the stone in the floor of your mouth during clinical examination. Depending on the size of the stone, and the location of it, your OMFS surgeon might be able to retrieve it through the duct of the gland, with the help of a camera and a basket, using a technique called endoscopic sialendoscopy (https://www.baoms.org.uk/patients/procedures/38/sialendoscopy).
If the stone is small and close to the floor of the mouth, is can be removed with a simple surgical procedure under local anesthetic. Occasionally, in cases of multiple or very large stones within the gland or at the hilum, require surgical excision of the submandibular salivary gland.
Sometimes, obstructive salivary gland disease can be due to very viscous saliva or debris instead of stones. Diagnosis is often difficult, as no investigation will show an obvious obstructive cause. However, patients usually improve after a sialogram, which might reveal no cause for the obstruction but it will wash out the debris and offer symptoms’ relief.
Autoimmune disorders
The most common autoimmune condition that affects the salivary glands is Sjögren’s syndrome. It occurs when the body’s immune system targets healthy cells in moisture-producing glands, such as the salivary, sweat, and oil glands. This condition most commonly affects women with autoimmune disorders, such as lupus or rheumatoid arthritis. The symptoms of Sjögren’s syndrome include dry mouth, dry eyes, joint pain or swelling, dry cough, fatigue and swollen salivary glands. Your OMFS surgeon might take a biopsy of your minor salivary glands from your lower lip, under local anesthetic. The treatment of Sjögren’s syndrome is medical; you should see and discuss it with your rheumatologist.
Investigations of salivary gland diseases
- Sialogram: This is a radiographic examination of the salivary glands ductal system. It involves the injection of contrast medium into the salivary duct of a single gland, followed by an X-ray. The contrast will highlight the ductal system and reveal areas of obstruction. Apart from diagnostic, it can occasionally be therapeutic, as the contrast medium washes out debris.
- Ultrasound scan: First line investigation for salivary gland lumps – it is also useful to guide fine needle aspiration (FNA)
- Fine Needle Aspiration: This is a form of biopsy, but instead of tissue sample, the OMFS H&N Surgeon samples few cells with the help of a syringe and needle. This is usually the case for lumps related to the salivary glands. The cells are viewed under a microscope to find out if they are abnormal.
- Core biopsy: This is similar to the FNA, but instead of a needle, a biopsy gun is used, that takes more tissue and allows for more confident histological diagnosis.
- MRI (Magnetic Resonance Imaging): A procedure that uses a magnet, radio waves, and a computer to make a series of detailed pictures of areas inside the body. An MRI of your salivary glands is very useful to outline benign and malignant tumours and help with the surgical planning.
- Occlusal dental X-ray: This is an X-ray of the floor of your mouth and can identify stones within the submandibular salivary gland duct.
Surgical Procedures
Parotidectomy:
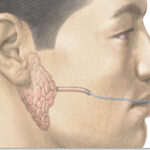
This procedure is the removal of the parotid salivary gland. Depending on the indication for surgery and the size of the tumour, your OMFS surgeon might remove all or part of the superficial portion of the parotid gland (superficial parotidectomy), all of the parotid gland (total parotidectomy) or all the parotid gland and surrounding structures (radical parotidectomy). For benign salivary gland disease, a partial superficial parotidectomy is often employed (removal of part of the parotid salivary gland around the tumour). Total parotidectomy is reserved for cases of refractory chronic sialadenitis.
The procedure is carried out under general anaesthetic. Your OMFS surgeon will access the parotid salivary gland via a skin incision that starts in front your ear and curves down to your neck. A very important nerve (called the facial nerve) passes through the parotid salivary gland and separates it into deep and superficial portions. This nerve is identified and protected during a parotidectomy, and every effort is made to preserve it intact in any parotidectomy done for benign disease. Nerve monitoring is used throughout the procedure.
Following the removal of the tumour and the required part of the parotid gland, the wound is closed and a drain is placed, usually for 24h. The patient is usually discharged home the next day. The skin sutures are usually removed in a week.
Possible complications
Like any other surgical procedure, the parotidectomy has potential risks. Your OMFS surgeon will discuss these risks prior to your surgery, so that you can make an informed decision, weighing the potential benefits of having the procedure versus the risks. The most common complications are:
- Facial nerve weakness
Dissection around the facial nerve can cause bruising or injury to the nerve, which will manifest with weakness of the same side of the face. The facial nerve has five main branches that are distributed in the facial muscles; therefore the weakness might be global or limited to one or more of the branches. You may not be able to lift your forehead or eyebrows, close your eyes tight, smile, puff up your cheek or you may notice droopiness on the angle of your mouth. The weakness might be partial or complete, and is measure using the House Brackmann scale (https://sorensenclinic.com/microsurgery/house-brackmann). Temporary weakness of the facial nerve that resolves within few weeks or few months is quite common, up to 25% of parotidectomies. However, permanent weakness is very rare, around 2%.
- Earlobe numbness
The nerve that provides sensation to the earlobe (greater auricular nerve) can be bruised during a parotidectomy procedure, and this results in (usually temporary) numbness of the earlobe.
- Infection
- Bleeding
- Sialocele
A Sialocele is a collection of saliva that can occur after parotid surgery. This is due to the fact that the cut remaining parotid salivary gland leaks saliva in the area of the operation, which collects and presents as a fluctuant swelling. It can be aspirated and it is usually self-resolving. However, persistent cases might need treatment with intraparotid Botox injections (https://medicine.uiowa.edu/iowaprotocols/botulinum-neurotoxin-treatment-salivary-gland-disorders).
- Frey’s syndrome
This is a very interesting entity and it comprises of sweating in the skin of the preauricular region every time the patient has a meal, following a parotidectomy procedure. It is due to cross-innervation of the cholinergic parasympathetic salivary gland nerve fibres with the sweat glands of the skin in that area. It can be annoying for the patients, and it is quite common. Treatment is with Botox injections, and is usually very successful (https://tinyurl.com/freysynd).
Submandibular gland excision
This is the procedure to remove the submandibular salivary gland. It is indicated in the treatment of malignant and benign tumours, in cases of recurrent sialadenitis, and in cases of obstructive sialolithiasis that the stone(s) can’t be removed with less invasive procedures.
The procedure is done under general anaesthetic. Your OMFS surgeon will access the gland via an incision in one of your neck creases, under your jawline. Following removal of the gland, you will be able to go home the same day. The skin sutures are usually removed in a week.
Possible complications
Like any other surgical procedure, the excision of the submandibular salivary gland has potential risks. Your OMFS surgeon will discuss these risks prior to your surgery, so that you can make an informed decision, weighing the potential benefits of having the procedure versus the risks. The most common complications are:
- Bleeding
- Infection
- Scarring
- Nerve damage
There are 3 nerves that lie within the operating field of this procedure and might be bruised or injured during this procedure. The first is the lingual nerve that provides sensation and carries taste fibers for the anterior two thirds of half of the tongue (on the same side). Bruising or injury to that nerve can cause numbness or tingling to half of the tongue and there is also a risk of altered taste. The second nerve is the marginal mandibular branch of the facial nerve. Bruising or injury to that nerve can cause droopiness of the lower lip on that side. The third nerve is the hypoglossal nerve that moves the tongue. Bruising or injury to that nerve can cause deviation of the tongue to the side of the surgery, and difficulties in speech and eating. The change of long-term nerve problems is extremely low. Any temporary weakness resolves within few weeks.
Sublingual gland excision
This is the procedure to remove the sublingual salivary gland. The most common indication is a ranula or a plunging ranula. Rarely, the sublingual gland needs to be removed for benign (very rare) or malignant tumours (usually as part of major oncological resection).
The procedure is done under general anaesthetic. Your OMFS surgeon approaches the sublingual gland through an intraoral cut in the floor of your mouth. Following the removal of the gland, you will have dissolvable sutures to close the wound. You can go home the same day.
Possible complications
Like any other surgical procedure, the excision of the sublingual salivary gland has potential risks. Your OMFS surgeon will discuss these risks prior to your surgery, so that you can make an informed decision, weighing the potential benefits of having the procedure versus the risks. The most common complications are:
- Bleeding
- Infection
- Injury to the lingual nerve
The lingual nerve provides sensation and carries taste fibers for the anterior two thirds of half of the tongue (on the same side). It runs in close proximity to the sublingual salivary gland, and can be injured during the procedure to remove the gland. Bruising or injury to that nerve can cause numbness or tingling to half of the tongue and there is also a risk of altered taste. This is usually temporary
- Injury to the duct of the submandibular salivary gland
The submandibular salivary gland duct runs in close proximity to the sublingual salivary gland, and can be injured during the procedure to remove the gland. This can result in stenosis of the gland and recurrent episodes of obstructive sialadenitis. It is usually self-limiting and the gland atrophies, but rarely it may require excision of the submandibular salivary gland to control the symptoms
Excision of mucocele
Mucoceles are common on the lower lip. The procedure to remove them is simple and done under local anesthetic. Your OMFS surgeon will inject and numb the area on your lower lip, and excise the mucocele. He will also remove the responsible minor salivary gland. You will have dissolvable sutures to close the wound. Possible risks include recurrence of the mucocele and temporary numbness to the lower lip.