Reconstructive surgery
Dr. Kyzas is the only OMFS H&N surgeon in Cyprus that offers personalized and holistic Head and Neck reconstructive surgery
- Reconstructive surgery – definition
- Why is it important for head and neck surgery
- Surgical techniques
What is reconstructive surgery?
Reconstructive surgery is a combination of skills and techniques that aim to rebuild and repair defects, in an attempt to restore appearance, cosmesis and function. In H&N surgery is mainly used to repair defects following ablative surgery for cancer. However, it’s also applied in severe traumatic defects and infections, and congenital conditions (i.e. clefts and craniofacial anomalies).
Using a wide variety of reconstructive techniques, Dr. Kyzas mends holes, repairs defects and restores function, in your mouth, face, scalp, neck (anywhere in the H&N region) primarily through the transfer of tissue from one part of the body to another. In addition to restore form and function, this type of surgery also aims to improve and restore appearance
Why is reconstructive surgery important for head and neck surgery?
The face of a person is the center of its soul; the mirror of everyone’s personality. Several vital functions initiate and end in the H&N area: Speech and talking, breathing, facial expression, smell, hearing, vision, swallowing, eating, and salivating. Our facial appearance is central to our lives; we smile, we cry, we kiss, we socialize.
Anything that distorts these vital functions has a profound functional, social and psychological impact. For any of us, the inability to eat, drink, talk, and socialize, is detrimental for the quality of our lives.
However, there are several conditions that result in such defects. For H&N Surgery, this is mainly the treatment for H&N cancer: the surgery that is required to treat and cure your cancer also results in significant defects that require expert reconstruction; and this is what Dr. Kyzas and his team aims to offer.
Head and Neck Conditions needing reconstruction
- H&N Cancer
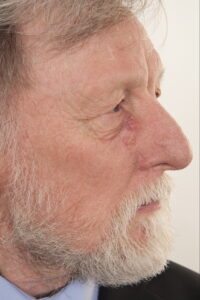
- Cutaneous (skin) cancer in the face, scalp, neck
- Vascular anomalies
- Cleft lip and palate
- Craniofacial defects (craniosynostosis)
- Trauma (severe forms, often with tissue loss)
- Aggressive forms of infection (i.e. necrotizing fasciitis)
- Burns
Surgical techniques
Head and neck reconstructive surgery is a challenging domain. Training is long and demanding, and cases are difficult and diverse. It’s a continually evolving area, with new techniques developing, aiming to improve the quality of life for patients. Dr. Kyzas has been a pioneer in personalized H&N reconstructive surgery (PSP), using 3D printing technology. He has led his unit in Manchester to become the largest unit in the UK offering this service. He has given several invited lectures on the topic. This has revolutionized the way we think about H&N reconstruction.
In a nutshell, reconstructive surgery involves the movement of large pieces of several types of tissue around the body.
The main revolution in reconstructive techniques occurred towards the end of the previous century, when surgeons applied microvascular surgery to allow transfer of tissue attached to its blood supply form one part of the body to others. This is called “free flap surgery” and it is the gold standard of H&N reconstruction.
The main reconstructive techniques
Skin grafts
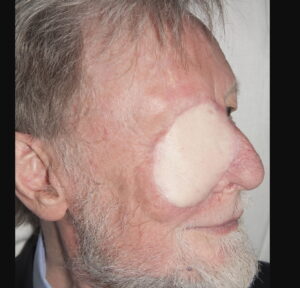
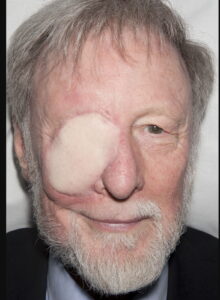
A skin graft is a piece of skin taken from another part of the body and transferred in the area of the wound defect. It gradually takes its blood supply from the tissues at the bed of the wound. It can be full thickness (contains the epidermis and all of the layers of the dermis) or split thickness (contains the epidermis and part of the dermis). When a split thickness skin graft is harvested (usually from the upper inner arm, the thigh, or the buttock) it leaves a graze that heals on its own in few weeks. On the other hand, harvesting a full thickness skin graft allows closure of the donor site in a straight suture line. Full thickness skin grafts are most commonly used in facial skin reconstruction. Donor sides include the abdomen, the thigh, the neck, around the ear, and the forehead. Occasionally, grafts can be composite. These are used to treat wounds that have a complex contour (i.e. after removal of a skin cancer from the nose). Composite grafts comprise all layers of skin, fat and sometimes the underlying cartilage from the donor site.
Tissue expansion
Tissue expansion is a procedure that enables the body to ‘grow’ extra skin by stretching surrounding tissue. A balloon-like device called an expander is inserted under the skin near the area to be repaired, and is then gradually filled with water, causing the skin to stretch and grow.
Flaps
Flap reconstruction involves the transfer of a living piece of tissue from one part of the body to another, along with the blood vessel that keeps it alive. Unlike a skin graft, flaps carry their own blood supply so can be used to repair larger and more complex defects.
- Local flaps
A local flap consists of mobilising tissue from areas adjacent to the defect, in a planned and often geometrical way, in order to facilitate wound closure under no tension and place the scars in the least visible areas (particularly important when it comes to the face). There are several types of local flaps, and your OMFS H&N surgeon will discuss the options with you. Local flaps use the principles of advancement, transposition and rotation.
- Regional flaps
A regional flap consists of mobilizing tissue from an area distally (but close) to the defect, and transferring it attached to its blood supply. Examples of regional flaps used in H&N reconstruction are the pectoralis major flap, the deltopectoral flap, and the supraclavicular island flap. Regional flaps are limited as to how far they can be transferred, and their blood supply isn’t consistent in all of the areas of the flap. They are however, extremely good options for specific indications.
- Free flaps/microvascular tissue transfer
The terms free flap and free tissue transfer are used to describe the movement of tissue from one site of the body to another. “Free” implies that the tissue is detached from the original location and then transferred to another location, along with its blood supply. The blood vessels are then reconnected (anastomosed) with donor vessels at the recipient site, with the help of the operating microscope. This is a highly complex surgical procedure, requiring extreme skills, but once successful, it offers unlimited reconstructive options to the head and neck surgeon.
The ability to disconnect and reattach tissue in this way means that the reach of flap is no longer confined by a patient’s anatomy.
Microvascular free tissue transfer has revolutionized H&N surgery more than any other technique. It is now the definitive treatment option and the gold standard of care for patients with H&N cancer.
In H&N surgery, free flaps can be simple or composite. Composite free flaps include more than one type of tissue (i.e. bone, muscle, skin, or combinations). Below there are few examples of the most commonly used free flap for H&N reconstruction
- Radial Forearm free flap (link to my course chapter)
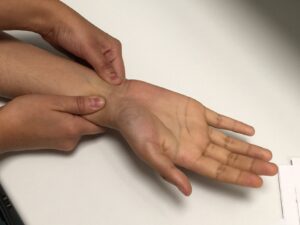
This flap is the workhorse of soft tissue H&N reconstruction. It involves taking skin and fascia from the forearm, attached to the radial artery (after ensuring adequate remaining blood supply to the hand with the Allen’s test.
This flap can be also be composite with the inclusion of bone, nerve, muscle, or even tendon. It has a wide range of applications, including reconstruction of the tongue, floor of the mouth, palate, pharynx, and many more. It is pliable, reliable, versatile, and has a long vascular pedicle. The donor site requires closure with a full thickness skin graft, often taken from the abdomen.
- Latissimus Dorsi free flap
This flap consists of skin and muscle taken from the back. It can provide large volumes of soft tissue, to reconstruct significant defects (i.e. skill base, total glossectomy, composite resections). It has the longest vascular pedicle available in the body and is an extremely reliable flap. Apart form its applications to H&N reconstruction; it is also used in breast reconstruction. It can be part of a composite flap, employing the entirety of the scapula system (including bone from the scapula – shoulder blade), in the form of a chimeric free flap.
- ALT free flap (anterolateral thigh)
This flap is a fasciocutaneous perforator flap (based on a small vessel that originates from the vascular pedicle and perforates through the fascia). The feeding vessel is the descending branch of the lateral circumflex femoral artery. It can provide large amounts of skin, and is particularly useful in reconstructing lateral skull base defects, due to the great skin colour match, and the opportunity to harvest a nerve graft (for facial nerve reconstruction/reanimation) at the same time of flap harvesting.
- Rectus abdominis flap
This flap includes taking skin and muscle form the anterior abdominal wall (your “six pack”). It is a bulky flap, largely depended on the body habitus, but is a great option for skull base defects’ reconstruction. It carries a risk of hernia development, therefore a mesh is used to re-enforce the abdominal wall after harvesting
Other types of soft tissue free flaps used in H&N reconstruction include:
- Lateral Arm Flap
- MSAP flap
- Gracilis flap (particularly for facial reanimation)
- DIEP flap
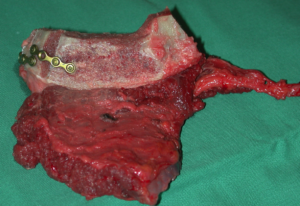
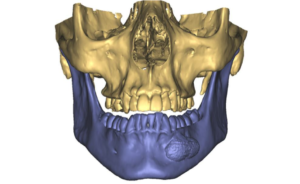
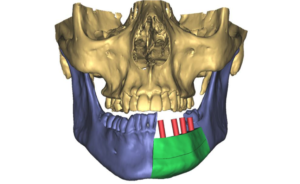
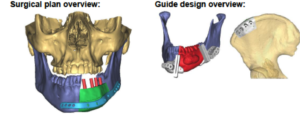
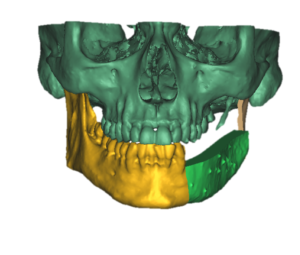
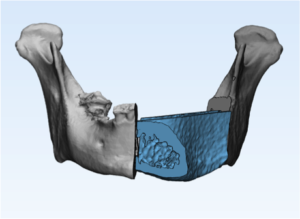
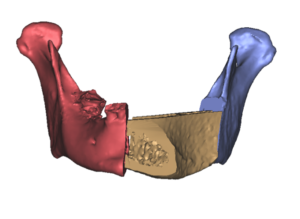
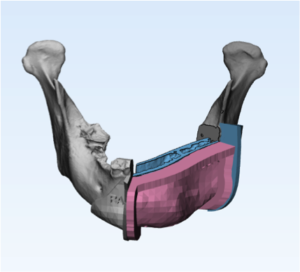
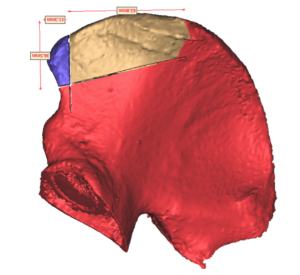
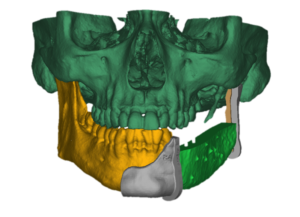
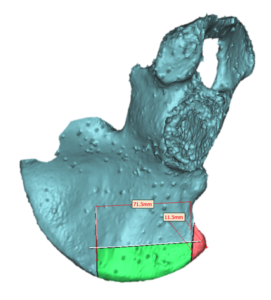
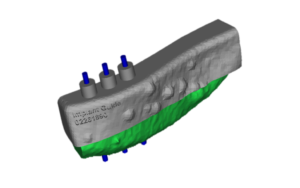
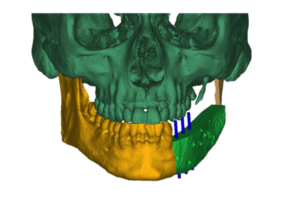
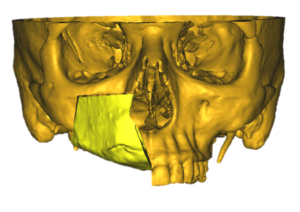
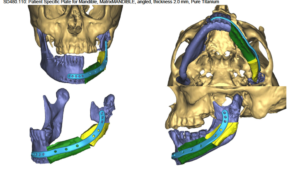
The greatest advancement in H&N surgery is the development of bony free flaps to reconstruct the bony structures of the face (mainly mandible and maxilla). With the use of 3D printer technology, these free flaps can be designed and guided to match the defect in a personalised way. The most common bony free flaps used in H&N reconstruction are:
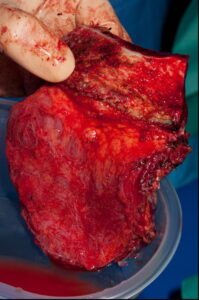
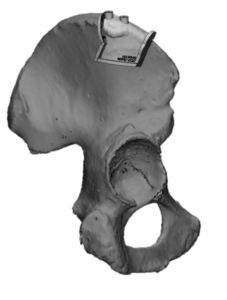
- DCIA free flap
This is a flap that includes bone from your hip (iliac crest). It is often combined with muscle (internal oblique) that provides the soft tissue lining. It provides excellent match for both mandible and maxillary reconstruction, and it allows dental rehabilitation with dental implants.
It is the flap of choice when it can be used. It carries a risk of hernia development, therefore a mesh is used to re-enforce the abdominal wall after harvesting. It has a relatively short vascular pedicle, but this is overcome with 3D modelling and planning.
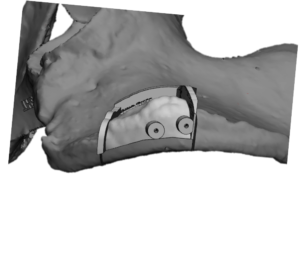
- Fibula Free flap
This flap includes harvesting your fibula bone, which a vestigial organ (like your appendix, you don’t need your fibula for function). It can be harvested with skin and can provide a long piece of bone, which is ideal for long bony defects (i.e. total mandibulectomy). The height of this flap is low, and dental rehabilitation with implants is difficult. It requires an angiogram to ensure that the blood supply to the foot won’t be compromised after the harvest.
- Scapula free flap
The scapula edge (shoulder blade) can provide bone for H&N reconstruction. The length and thickness of the bony part of this flap is limited, however, it is the flap of choice when the required soft tissue defect is large. It can be combined with lots of soft tissue, i.e. in the form of a chimeric flap with latissimus dorsi. With the use of 3D technology, it in now possible to harvest this flap in a way that will allow dental rehabilitation with implants.
Other types of bony free flaps that are rarely used include:
- Composite radial free flap
- Femur flap
- Humerous flap
- Serratus anterior + rib
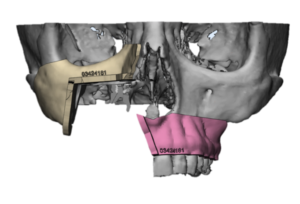
3D planning and PSP reconstruction
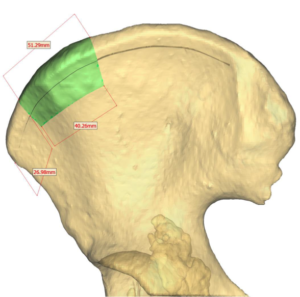
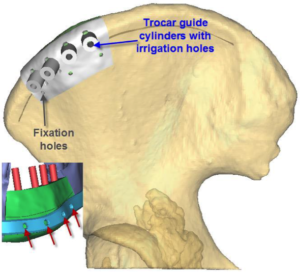
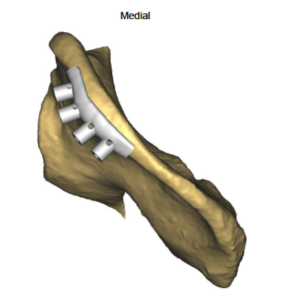
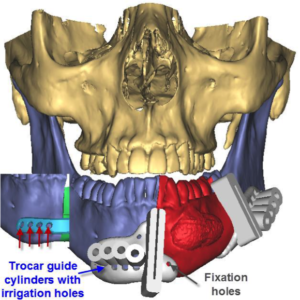
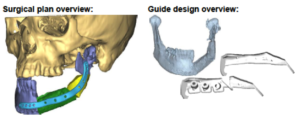
The biggest difficulty in H&N bony reconstruction is to get the shape and size of the bone to accurately fit the size of the surgical defect, and to make it amenable to accept dental implants for dental rehabilitation. In addition, the adaptation of metal plate that holds everything together is often difficult, and can if not perfect, it can result in implant fatigue, loose screws and extrusion of the plate through the mouth or the skin of the neck.
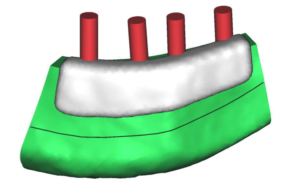
Therefore, 3D printer technology is now employed, to plan bony resections and reconstructions. An acrylic model of the donor and the recipient side is made, and cutting guides are designed both for the resection of the tumour and the harvesting of the flap. The metal plate is then milled or pre-bend based on those guides. The overall result is as close to perfection as surgery can get it.
Dr Kyzas has been a pioneer in the UK in developing and expanding this technique. It should be considered as the gold standard of H&N bony reconstruction and it can now be provided in Cyprus.
Useful links