Orthognathic Surgery
Overview
Orthognathic surgery (from the Greek words Ορθός + Γναθος, straight jaws) is the surgical treatment of repositioning and refashioning the upper, lower, or both jaws, in a more aesthetically pleasing and functional position. It is used in combination with orthodontic treatment, in patients who have a large discrepancy between the size of the jaws in relation to each other, or the jaws have grown in an abnormal position in relation to the surrounding structures (i.e. base of skull)
Patients with anomalies of the jaw usually present with malocclusion (poorly aligned teeth), which requires joint assessment by an orthodontist and an OMFS surgeon. Jaw size/position discrepancies are common, and sometimes the patients have significant facial deformity. As a result, the function of the jaws and the quality of life of these patients is compromised in many ways:
- Difficulty eating
- TMJ problems and muscle pain
- Speech difficulties
- Damage to the gums due to a wrong, often traumatic bite
- The facial appearance is compromised, and this leads to psychological distress which affects interpersonal relationships
Causes of jaw discrepancy
In the majority of cases, there is no specific cause; the discrepancies are simply the way the jaw has grown. There might be a family history. Childhood jaw trauma has been linked to jaw discrepancies. Congenital abnormalities, like cleft lip or palate are associated with maxillary hypoplasia, whereas some syndromes such as hemifacial microsomia are linked with mandibular hypoplasia. In general, congenital and syndromic cases are the rarity.
Jaw discrepancies are usually detected during puberty, most of the times in an appointment with the orthodontist, as the “teeth are not well aligned”. Corrective Orthognathic Surgery should be done once jawbone growth is complete which happens usually in late adolescence.
Why is Orthognathic surgery beneficial?
- The function of the teeth, jaws and mouth can be improved (which results in better eating, speaking and confidence).
- Improvement in facial and dental appearance
- Improvement in psychology and quality of life
Treatment outline
- Planning (close communication and/or joint consultation with orthodontist and OMFS surgeon)
- Orthodontic preparation
- Surgery
- Final orthodontic treatment
Planning
Patients with jaw discrepancies are usually firstly seen and diagnosed by their orthodontist. He will discriminate between a purely dental cause for the patient’s malocclusion and an underlying skeletal anomaly. At this stage a diagnosis is made and the patient referred to the OMFS surgeon, who will further examine and assess the patient. The OMFS surgeon and the orthodontist will formulate the treatment plan jointly. Throughout the treatment, your OMFS surgeon and your orthodontist will be in close communication.
It is important to stress that any orthognathic surgery should be delayed until jaw growth is complete (at approximately 16-18 years of age).
Investigations
A number of investigations are required at this stage. These include radiographs (OPG and Cephalometric), models of the teeth, and facial and dental photographs.

A computer planning software will simulate the proposed jaw and teeth movements (https://www.dolphinimaging.com/product/ThreeD?Subcategory_OS_Safe_Name=3D_Surgery). Special splints, called the wafers, will be made, to aid the OMFS surgeon during surgery. Recently, 3D printer technology and surgical guides have been used in orthognathic surgery, implementing the knowledge gained by the use of this technology in H&N reconstruction (link to my reconstruction page). The results are excellent.
Orthodontic preparation
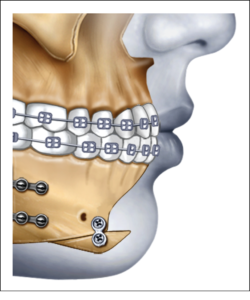
Orthodontic braces fixed to the teeth are necessary to straighten the teeth so that the two jaws can ‘fit’ together properly during surgery. This stage can either be short (in which case a longer period of braces is required after surgery), or longer, so that minimal orthodontic adjustments are needed after surgery). It can take between 12 – 18 months.
Surgery
Following the orthodontic preparation, your OMFS surgeon and your orthodontist will have prepared surgical guides, wafers and simulate the jaw movements on computer software. Your OMFS surgeon will explain the details of the procedure and mention the possible risks and complications so that you can make an informed decision.
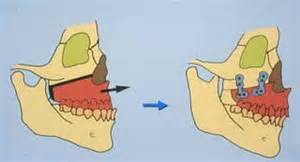
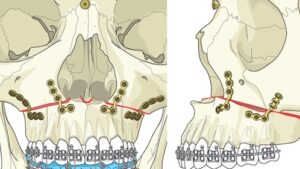
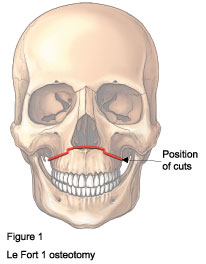
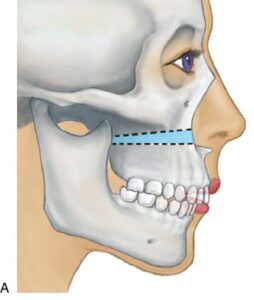
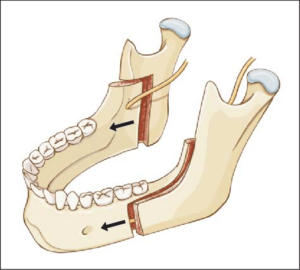
In general, the operation involves surgical cut (break) of the upper or the lower jaw, or both. Occasionally, an operation to correct the chin, called a Genioplasty, is done at the same time. Most common maxillary procedure is the LeFort I osteotomy and for the mandible is the sagittal split ramus osteotomy.
The operation is carried out under general anaesthesia. The incisions to expose the bones are made inside the mouth (no facial scars). Once the jaw(s) are cut they are moved to the desired pre-planned position and are fixed in place using titanium miniplates and screws.
You would expect to stay in the hospital for 1-2 days following this procedure. Full recovery usually takes 3-4 weeks.
Final orthodontic treatment
Following surgery, the orthodontist makes any required adjustments to the teeth alignment. How much orthodontic treatment will be needed depends on the extent of the pre-surgical orthodontic preparation.
Possible complications
Like any other surgical procedure, orthognathic surgery has potential risks. Your OMFS surgeon will discuss these risks prior to your surgery, so that you can make an informed decision, weighing the potential benefits of having the procedure versus the risks. The most common complications are:
- Nerve damage: The inferior dental nerve travels within the lower jaw, and the infraorbital nerve is very close to the bone cut for the upper jaw. These nerves can be bruised or damaged during orthognathic surgery. You may experience numbness or tingling to the lips, chin, cheeks, gums and teeth. In most cases, this is transient and resolves within few weeks. However, in some cases, it can be prolonged or permanent.
- Bleeding
- Infection
- Damage to the teeth
- Relapse: Some jaw movements are more stable than others. Rarely, it is possible for the teeth and jaws to tend to move back towards their original position, mainly due to muscle pull and contraction of the healing soft tissues. Orthodontic retainers may need to be used.
Useful links
- https://www.baoms.org.uk/patients/procedures/26/maxillary_upper_jaw_osteotomy
- https://www.bos.org.uk/Portals/0/Public/docs/PILs/OrthognathicTreatmentJuly2016V1.pdf
- https://www.thefacesurgeons.co.uk/treatments/jaw-surgery/maxillary-osteotomy/
- https://www.ucc.ie/en/media/academic/dentalschool/patientinfoleaflets/Orthognathic(Jaw)Surgery.pdf