General Information About Oropharyngeal Cancer
- Oropharyngeal cancer is a disease in which cancer cells develop form in the tissues of the oropharynx.
- Smoking or being infected with human papillomavirus can cause oropharyngeal cancer.
- Signs and symptoms of oropharyngeal cancer include a lump in the neck and a sore throat.
- HPV – related oropharyngeal cancer carries excellent prognosis and is now considered as different disease
Oropharyngeal cancer is a disease in which cancer cells develop form in the tissues of the oropharynx.
The oropharynx is the middle part of the throat, behind the mouth. It starts behind the nose and ends where the larynx (voice box) and esophagus (gullet) begin. Air and food pass through the pharynx on the way to the larynx or the esophagus.
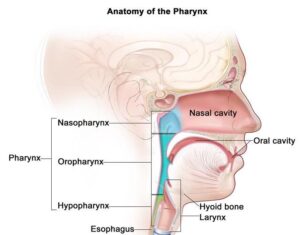
The oropharynx includes the following:
- Soft palate.
- Side and back walls of the throat.
- Tonsils.
- Base of the tongue (back 1/3).
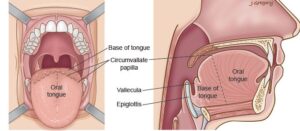
Oropharyngeal cancer is a type of head and neck cancer. Like mouth cancer (link) most of cancers in the oropharynx are squamous cell carcinomas.
Smoking or being infected with human papillomavirus can cause oropharyngeal cancer.
The most common risk factors for oropharyngeal cancer include the following:
- Smoking (any form; cigarettes, pipe, shisha)
- Heavy alcohol use.
- Being infected with human papillomavirus (HPV), especially HPV type 16.
Signs and symptoms of oropharyngeal cancer
These and other signs and symptoms may be caused by oropharyngeal cancer or by other conditions. Check with your doctor if you have any of the following:
- A sore throat that does not go away
- Difficulties in swallowing
- Trismus (not being able to opening the mouth fully)
- Difficulties in moving the tongue or speech
- Weight loss
- Earache
- A lump in the back of the mouth, throat, or neck
- A white patch on the tongue or lining of the mouth that does not go away
- Coughing up blood
Sometimes oropharyngeal cancer does not cause early signs or symptoms and can indolently present with a single neck lump
Examination, diagnosis, investigations
- Clinical examination and history: Your OMFS H&N surgeon will ask about your social habits (smoking and drinking) and take a thorough medical history. He will exam the lips and oral cavity looking for anyabnormal Your OMFS H&N Surgeon will look carefully and feel the entire mouth with a gloved finger and examine the oral cavity with a mirror and good light. The neck will be felt for swollen lymph nodes.
- Fiberoptic nasoendoscopy: If needed, your OMFS H&N surgeon will pass a thin tube-like camera through your nose, to examine the back of your throat, the base of your tongue and your voice box (larynx).
- Biopsy: This is paramount in order to diagnose cancer. Your OMFS H&N Surgeon will take a sample of the abnormal area, usually under local anaesthetic, and send it to be viewed under a microscope by a pathologist. Given the difficulty in getting to this particular area of the throat, you may need to have an EUA (Examination Under Anaesthesia)
- Fine Needle Aspiration: This is a form of biopsy, but instead of tissue sample, the OMFS H&N Surgeon samples few cells with the help of a syringe and needle. This is usually the case for lumps in the neck (lymph nodes). The cells are viewed under a microscope to find out if they are abnormal.
- MRI(Magnetic Resonance Imaging): A procedure that uses a magnet, radio waves, and a computer to make a series of detailed pictures of areas inside the body. An MRI of your H&N region is required to stage the cancer

- CT scan F5: A computerised x-ray that makes a series of detailed pictures of areas inside the body, taken from different angles. A CT scan of your thorax (chest) is needed for staging H&N cancer, to exclude disease spread and/or second primaries in the lung

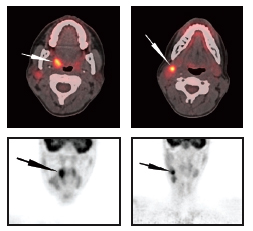
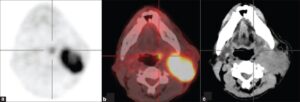
- PET scan (positron emission tomography scan): A procedure to find malignanttumour cells in the body. A small amount of radioactive glucose (sugar) is injected into a vein. The PET scanner takes picture of where glucose is being used in the body. Malignant tumour cells show up brighter in the picture because they are more active and take up more glucose than normal cells do. The PET scan is particularly useful when the cancer present as an isolated neck lump and the primary tumour is very small (usually hidden in the base of the tongue or the tonsils)
- EUA (Examination Under Anaesthesia): For this exam, you will be asleep. Your OMFS H&N surgeon will thoroughly examine the areas of your throat and take samples from abnormal looking areas. Occasionally (especially in cases of neck occult primary) your surgeon might need to sample areas of your tongue base and remove your tonsils, even if they look normal, as the primary cancer might be very small and indolent
- HPV test(human papillomavirus test): A laboratory test used to check the sample of tissue to check whether your cancer is caused by HPV
Factors affecting the outcome
The prognosis (chance of cure and recovery) depends on:
- Whether the cancer is HPV related
- Whether the patient is/was a smoker.
- The stage of the cancer.
- The location of the cancer.
Oropharyngeal tumours related to HPV infection have a better prognosis and are less likely to recur than tumours not linked to HPV infection.
Treatment options depend on the following:
- The stage of the cancer.
- The size and the location of the tumour.
- The patient’s general health.
Patients who have oropharyngeal cancer have an increased risk of developing a second cancer in the head or neck, or a synchronous cancer in the lung. Frequent and careful follow-up is important
Stages of oropharyngeal Cancer
- HPV oropharyngeal cancer is staged differently than non-HPV oropharyngeal cancer
- There are three ways that cancer spreads in the body.
- Cancer may spread from where it began to other parts of the body.
- The following stages are used for oropharyngeal cancer:
- Stage 0 (Carcinoma in Situ)
- Stage I
- Stage II
- Stage III
- Stage IV
The way oropharyngeal cancer is staged is complex – your OMFS H&N surgeon will explain the stage and the implications once all tests are completed.
The process used to find out if oropharyngeal cancer has spread to other parts of the body is called staging. Staging guides decision-making and treatment.
There are three main ways that cancer spreads in the body.
Cancer can spread through tissue, the lymph system, and the blood:
- The cancer spreads from where it began by growing into nearby areas.
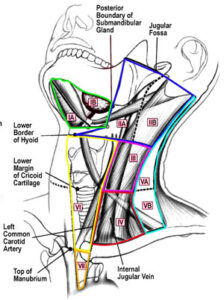
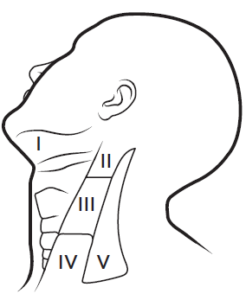
- Lymph system. The cancer spreads to the lymph glands (in H&N cancer it spreads in the neck lymph glands).
- The cancer spreads from where it began by getting into the blood. The cancer travels through theblood vessels to other parts of the body (distant metastasis).
When cancer spreads to another part of the body, it is called metastasis.
Treatment
- Because HPV-related oropharyngeal cancer carries good prognosis, every effort is made to reduce the morbidity of treatment
- Radiotherapy with or without chemo is the first line treatment for oropharyngeal cancer where surgery cannot be performed or is deemed too morbid
- Recent advances in surgery (transoral Laser resection – TOLS and Transoral Robotic resection – TORS) are increasingly used
- Patients with oropharyngeal cancer should have their treatment planned and delivered by a team who is expert in treating head and neck cancer.
- Two types of standard treatment are used:
- Surgery(best offered from surgeons experienced in TOLS or TORS)
- Radiation therapy
- Chemotherapy(only in selected cases and as adjunct to radiotherapy)
- Treatment for oropharyngeal cancer is difficult, complex and may cause side effects.
- Follow-up tests may be needed.
Patients with oropharyngeal cancer should have their treatment planned by a team of doctors who are expert in treating head and neck cancer.
Your expert OMFS/H&N Surgeon, who will guide the team for you, will oversee your treatment. The oropharynx (throat), neck and face are vital areas for eating, drinking, talking, cosmesis and psychology. A team approach is required to overcome the potential side effects of the treatment. The team usually include:
- Head and necksurgeon (ablation and reconstruction)
- Radiation oncologist
- Speech therapist
- Dietitian
- Pathologist
- Radiologist
- CNS
Surgery
Surgery (removing the cancer in an operation) can be considered when appropriate. Surgery might include the following:
- TOLS or TORS resection of the primary tumour: With this technique, your OMFS H&N Surgeon will use laser or a robot, to remove the primary cancer from areas that are difficult to access otherwise. This is a difficult technique that requires extensive training and skill; but it has very low morbidity and in most cases doesn’t need reconstruction of the surgical defect. It is suggested that it might lead to better swallowing compared to traditional treatment modalities
- Wide local excision of the primary tumour: Removal of the cancer and some of the healthytissue around it. This can be used in cases of HPV – negative soft palate cancers, or in previously treated oropharyngeal cancer that recurs (salvage surgery)
- Neck dissection: Removal oflymph nodes in the neck. This is done when cancer has or may have spread from the lip and oral cavity. This also provides access to blood vessels for microvascular reconstruction.
- Reconstruction: In cases that the cancer cannot be removed with TOLS or TORS, and open surgery is indicated, your OMFS Surgeon will discuss reconstruction options with you. This is a highly demanding and highly important part of oropharyngeal cancer treatment. The defect created by the removal of the tumour needs to be re-build to improve appearance and function and reduce the risk of potential side effects. The gold standard is the use of microvascular free tissue transfer (the surgeon takes tissue – skin, muscle, bone, or combinations – from other parts of the patients’ body, preserving the blood vessels and re-perfuses the flap by anastomosing the blood vessels with donor vessels in the neck. This is called microvascular surgery and it is done under the operating microscope. Offering this kind of treatment should be the minimum you would expect from your OMFS H&N Surgeon.
Radiatiotherapy
Radiatiotherapy is a cancer treatment that uses high-energy radiation to kill cancer cells or keep them from growing. It is usually given after the surgery, depending on specific indications, and is called adjuvant therapy. Occasionally, in the event of residual tumour after surgery or if there is disease in the neck glands with extracapsular spread (ECS), radiotherapy will be given combined with chemotherapy, to increase its efficacy. For oropharyngeal cancers, it can be used alone or in a combination with chemotherapy as the single required treatment.
Side Effects
Treatment for mouth cancer is difficult and can result in life-changing side effects. Your OMFS H&N surgeon will follow you up and try to deal with these side effects whenever possible
- Xerostomia – dry mouth
- Difficulties in speech
- Difficulties in swallowing (may require feeding tube)
- Changes in appearance
- Weight loss
- Infection
- Lymphedema
- Chronic pain
- Osteoradionecrosis (ORN)
- Shoulder dysfunction
- Taste changes
- Scarring