Malignant Melanoma
- Definition
- Causes
- Diagnosis
- Treatment
Definition
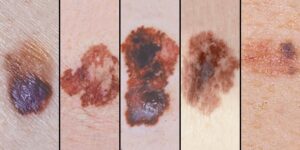
Malignant melanoma is a type of skin cancer. There are two main types of skin cancer: melanoma and non-melanoma skin cancer. Melanoma arises from the melanocytes in the skin (cells that produce melanin – a brown-black pigment/colour substance). In this cancer the melanocytes become malignant and multiply excessively.
Very often the first sign of a melanoma developing is a previous mole changing in colour or a new brown/black lesion developing.
Melanoma is the most serious type of skin cancer because it is more likely to spread (metastasise) from the skin to other parts of the body. Depending on the stage of the disease, it might be lethal
Causes
One of the most important causes of melanoma is exposure to too much ultraviolet light in sunlight. The use of artificial sources of ultraviolet light, such as sunbeds, also increases the risk of getting a melanoma.
Overexposure to ultraviolet (UV) light is one of the main causes of melanoma. UV light comes from the sun, as well as from artificial tanning sunbeds and sunlamps. A history of multiple sunburns also increases the risk, especially in fair skin individuals. Occasionally, melanoma develops in a previous mole that is changing in appearance.
Family history is important for melanoma development, and the risk increases with 3 or more relatives having had the disease. Other risk factors include:
- Fair skin or red hair
- A large number of moles
- Having a very large dark birthmark
- Immunosuppression
- Previous history of melanoma
Diagnosis
Lesions that look suspicious for melanoma should be excised with a narrow (2mm) margin (excisional biopsy). The specimen will be examined under the microscope by the pathologist. This will confirm or refute the diagnosis of melanoma and also give the thickness of the tumour, which is important for staging the disease. This is called Breslow thickness and measures how far the melanoma cells have invaded down into the layers of skin. Breslow thickness, and other information from the histology report will be used to satge the disease. You may also need to have specialist scans (like a PET-CT), to assess whether the disease has spread anywhere else in your body.
There are 4 stages for malignant melanoma (Stage 1 to Stage 4). Stage 1 is the earliest stage of the disease and most of the times it can be treated with an intention to cure it.
If you present with a melanoma on your face or your scalp, your OMFS H&N Surgeon will perform all the required diagnostic tests, and discuss your case with a team of experts in what is called a multidisciplinary meeting (MDT meeting). This normally includes (apart from your surgeon), oncologists, pathologists, radiologists, specialist nurses. They will be part of the team that will look after you.
Treatment
Treatment for malignant melanoma depends hugely on the stage of the disease. It could be as simple as wide local excision of the lesion, but it may also require a combination of surgery, radiotherapy, chemotherapy, or new forms of medical treatment (i.e. immunotherapy). In advanced stages, you may be offered the opportunity to participate in clinical trials that test new forms of treatment. Your surgeon will discuss the treatment options and the prognosis with you in detail.
Treatment can be challenging and complex when melanomas appear in difficult areas, such as the face. Your OMFS H&N surgeon will ensure that he adequately removes the skin cancer and reconstructs the wound respecting appearance and cosmesis.
When possible, surgery is the first line treatment for melanomas.
Wide local excision: This removes the melanoma with a margin of healthy looking (how much healthy tissue needs to be removed depends on the stage, and your surgeon will explain the details).
The surgery is usually done under local anaesthetic. Once the melanoma has been removed, the surgeon will reconstruct the wound. That might be as simple as closing the wound primarily with few stitches, but in the majority of cases, when it comes to the face, more complex reconstruction is needed to achieve the best cosmetic result. This is done in the form of a local skin flap or a skin graft
Local skin flaps
A local skin flap is mobilising skin from areas adjacent to the defect, in a planned and often geometrical way, in order to facilitate wound closure under no tension and place the scars in the least visible areas (particularly important when it comes to the face). There are several types of skin flaps, and your OMFS H&N surgeon will discuss the options with you (Photos).
Skin graft
A skin graft is a piece of skin taken from another part of the body and transferred in the area of the wound defect. It gradually takes its blood supply from the tissues at the bed of the wound. It can be full thickness (contains the epidermis and all of the layers of the dermis) or split thickness (contains the epidermis and part of the dermis). When a split thickness skin graft is harvested (usually from the upper inner arm, the thigh, or the buttock) it leaves a graze that heals on its own in few weeks. On the other hand, harvesting a full thickness skin graft allows closure of the donor site in a straight suture line. Full thickness skin grafts are most commonly used in facial skin reconstruction. Donor sides include the neck, around the ear, and the forehead.
Sentinel node biopsy

Patients with a stage 2 melanoma might benefit from a diagnostic procedure called a sentinel lymph node biopsy. The reason is that if a melanoma does spread, then it usually spreads to the nearest lymph gland (hence, “sentinel” node)
The first part of a sentinel lymph node biopsy involves injecting a radioactive liquid into the skin near to where the melanoma was located. A scan is then carried out to see which node or nodes the liquid reaches. This identifies the sentinel node
The second part of the test takes place at the time of the excision of the melanoma when the surgeon injects blue dye into the same place that the radioactive liquid was injected. This makes the node visible to the surgeon. The combination of the radioactive liquid and blue dye is the best way to identify the sentinel node. The surgeon removes that node and he sends it to the pathologist who will examine it for malignant melanoma cells spread.
The result is called positive if melanoma cells are found. Following that, the patient is usually offered lymph node dissection.
Neck dissection: When melanoma has spread to the regional neck lymph glands, or when the result of the sentinel node biopsy was positive, a procedure to remove the neck lymph glands is undertaken. This includes the removal of the lymph nodes in the neck, and occasionally it is combined with a parotidectomy (removal of the parotid salivary gland and the lymph nodes that it contains). This is done when the melanoma has spread from the face or scalp. This also provides access to blood vessels for microvascular reconstruction, in case the defect after the primary cancer excision is significant.
Other treatments include:
- Radiotherapy: The radiotherapy is used in advanced stages of the disease, to reduce or remove symptoms. It won’t cure melanoma. It is therefore given with palliative intention.
- Targeted Therapies
Some melanomas contain an altered gene (BRAF protein). After the biopsy, the pathology lab will look for this gene. If it is present then a targeted therapy, a drug called BRAF inhibitor may be given. This will not cure melanoma, but it may slow down disease progression. - Chemotherapy: Chemotherapy is the use of anti-cancer drugs to destroy cancer cells. In melanoma, chemotherapy is used to control/slow down the disease
- Immunotherapy: This treatment boosts your own body’s immune system to act against melanoma cells. A drug called Ipilimumab is used for melanoma and helps the cells in the body’s defence system to work more effectively.
- Clinical trials: Sometimes you might be eligible for experimental treatment that can create knew scientific knowledge of the disease and increase your chances of longer disease control.
Useful links
- https://www.nice.org.uk/guidance/ng14
- https://www.cancerresearchuk.org/about-cancer/melanoma/symptoms?_gl=1*kmwpnr*_ga*MTI5NTcwMzA5LjE2ODQ0NzcyODk.*_ga_58736Z2GNN*MTY5NzYxODk1NS4yLjEuMTY5NzYxODk4MS4wLjAuMA..*_gcl_au*MTkwNjc2Nzc1NS4xNjk3NjE4OTY4&_ga=2.232953117.2055077332.1697618956-129570309.1684477289
- http://www.macmillan.org.uk/Cancerinformation/Cancertypes/Melanoma/Melanoma.aspx