Basal Cell Carcinoma
- Definition
- Causes
- Diagnosis
- Treatment
Definition
A basal cell carcinoma (BCC) is a type of skin cancer. There are two main types of skin cancer: melanoma and non-melanoma skin cancer. BCC is a non-melanoma skin cancer, and is the most common type all skin cancers. BCCs are sometimes referred to as ‘rodent ulcers’ (Photo).
Causes
Overexposure to ultraviolet (UV) light is the main cause of non-melanoma skin cancer. UV light comes from the sun, as well as from artificial tanning sunbeds and sunlamps. BCCs can occur anywhere on the body, but are most common on areas that are exposed to the sun such as your face, head, neck and ears.
BCCs mainly affect fair skinned adults, but other skin types are also at risk. Those with the highest risk of developing a basal cell carcinoma are:
- People with pale skin who burn easily and rarely tan
- Those who have had a lot of exposure to the sun (i.e. fishermen, farmers)
- People who have used sun beds or have regularly sunbathed
- People who have previously had a basal cell carcinoma.
BCCs are not hereditary, apart from a rare familiar condition called Gorlin-Gotz syndrome
Diagnosis
The clinical appearance of these lesions is most of the times enough to characterise them. Your doctor will refer you to the OMFS H&N Surgeon for any lesion that looks abnormal on your face. Direct inspection or use of dermoscopy (looking at the lesion with a special magnifying glass) is often enough to diagnose the lesion.
BCCs can vary greatly in their appearance, but people often first become aware of them as a scab that bleeds and does not heal completely or a new lump on the skin. Some BCCs are superficial and look scaly. Others form a lump and have a pearl-like rim surrounding a central crater. If left untreated, BCCs can eventually cause an ulcer; hence the name “rodent ulcer”.
Rarely, a skin biopsy might be needed to confirm the diagnosis.
Treatment
BCCs can be cured in almost every case. They don’t spread to other parts of the body, they don’t metastasize, therefore, if treated properly, they are not life threatening.
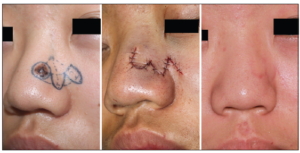
Treatment can be challenging and complex when BCCs appear in difficult areas, such as the face. Your OMFS H&N surgeon will ensure that he adequately removes the skin cancer and reconstructs the wound respecting appearance and cosmesis.
Surgery is the first line treatment for BCCs. Any other treatment options should be carefully considered only when surgery isn’t possible
Surgery with a predetermined margin is the main treatment for non-melanoma skin cancers. It involves removing the cancerous tumour and some of the surrounding skin (around 3-4mm, depending on the type and the area).
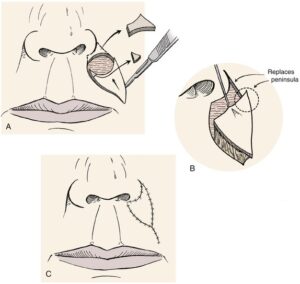
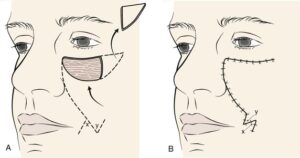
The surgery is usually done under local anaesthetic. Once the BCC has been removed, the surgeon will reconstruct the wound. That might be as simple as closing the wound primarily with few stitches, but in the majority of cases, when it comes to the face, more complex reconstruction is needed to achieve the best cosmetic result. This is done in the form of a local skin flap or a skin graft
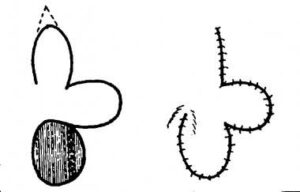
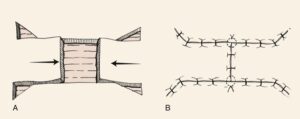
Local skin flaps
A local skin flap is mobilising skin from areas adjacent to the defect, in a planned and often geometrical way, in order to facilitate wound closure under no tension and place the scars in the least visible areas (particularly important when it comes to the face). There are several types of skin flaps, and your OMFS H&N surgeon will discuss the options with you.
Skin graft
A skin graft is a piece of skin taken from another part of the body and transferred in the area of the wound defect. It gradually takes its blood supply from the tissues at the bed of the wound. It can be full thickness (contains the epidermis and all of the layers of the dermis) or split thickness (contains the epidermis and part of the dermis). When a split thickness skin graft is harvested (usually from the upper inner arm, the thigh, or the buttock) it leaves a graze that heals on its own in few weeks. On the other hand, harvesting a full thickness skin graft allows closure of the donor site in a straight suture line. Full thickness skin grafts are most commonly used in facial skin reconstruction. Donor sides include the neck, around the ear, and the forehead.
Other treatments include:
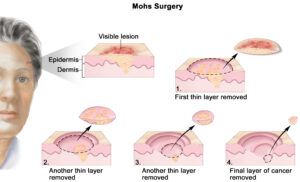
- Mohs micrographic surgery. This surgical procedure is used to treat more complex BCCs such as those present at difficult anatomical sites or recurrent BCCs. The procedure involves excision of the affected skin and examination of the skin removed under the microscope straight away to see if all of the BCC has been removed. This process continues until all of the BCC is completely removed. The wound is then assessed and reconstructed as above. This is a time consuming process and is only undertaken when simple surgery may not be suitable.
- Radiotherapy: Surgery and radiotherapy are the two modalities that are supported by strong medical evidence in the treatment of BCCs. However, radiotherapy is expensive and time consuming, and is mainly reserved for patients that cannot have surgery.
- Curettage and cautery.
- Cryotherapy: Freezing the BCC with liquid nitrogen.
- Anti-cancer creams:The two most commonly used are 5-fluorouracil (5-FU) and imiquimod.
- Photodynamic therapy: a special form of light treatment.
The treatment used will depend on the type, size and location of the BCC you have. Because facial skin cancer is in a difficult area of the body, your treatment should be carried out by a surgeon experienced is excision and reconstruction of such lesions.
Useful links
- https://www.bad.org.uk/pils/basal-cell-carcinoma/
- https://www.uhcw.nhs.uk/download/clientfiles/files/Patient%20Information%20Leaflets/Trauma%20and%20Neuro%20services/Plastics/Skin%20grafts.pdf
- https://www.skincancer.org/skin-cancer-information/basal-cell-carcinoma
- https://www.dermnetnz.org/topics/basal-cell-carcinoma/