Wisdom teeth
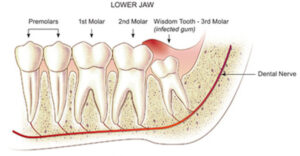
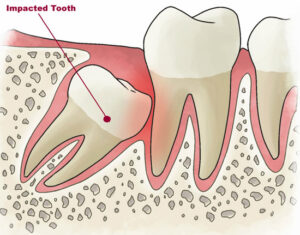
Wisdom teeth (third molars) are usually the last teeth to erupt through the gums. Most people have four wisdom teeth, although some people have less or none at all. Often, there is not enough space for the wisdom teeth to erupt through the gums. They either partially erupt or remain “impacted”. Some of the impacted wisdom teeth remain completely buried and cause no trouble whatsoever. However, other impacted wisdom teeth may cause severe problems and require surgical extraction.
Removal of a wisdom tooth or wisdom teeth is a very common procedure.
Potential problems caused by impacted Wisdom Teeth (indications to remove them):
- Recurrent infections (pericoronitis)
- Crowding: (your orthodontist might want your wisdom teeth removing to be able to align your teeth)
- Chronic pain
- Cysts: Often, impacted wisdom teeth are associated with a cyst (“dentigerous” cyst) that needs removing with the wisdom tooth
- Food trap: Food can become between between the wisdom tooth and the molar next to it. This can cause cavities or infection in both teeth.
- Resorption of the molar next to the wisdom tooth: An impacted wisdom tooth may continue pushing against the molar next to it. This can cause a resorption to the other molar. In order to save the molar tooth (if possible) the wisdom tooth needs to be extracted.
- Decayed wisdom teeth
Investigations
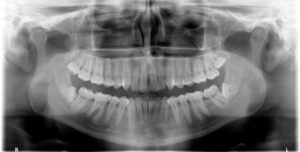
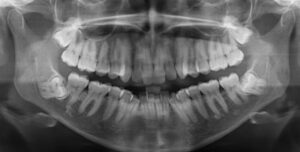
The most common X-Ray required is an OPG, which will show all the wisdom teeth, it will reveal signs of infection or other pathology, it will highlight the relation of the wisdom tooth to the adjacent molars and will show the proximity of the roots of the wisdom tooth to the inferior dental nerve.
Occasionally, a specialist CT scan, called cone beam CT, will be requested, to examine the relationship of the wisdom tooth roots with the nerve in great detail.
Treatment
Your OMFS surgeon will examine your mouth and teeth, take a full history and look at the x-rays and the rest of the investigations. He will then recommend whether you require extraction of all or some of your wisdom teeth.
Wisdom Teeth extractions in young age
In young people, the roots of the wisdom teeth are not completely formed, and the surrounding bone is softer. This allows for easier extraction of the tooth. Therefore, your OMFS surgeon will assess and offer extraction of wisdom teeth in young patients, if there are appropriate indications.
Surgical Procedure
- Local anesthetic: Your OMFS surgeon will inject local anesthetic which will numb the gums and parts of your face. It wears off within few hours
- Removal of Wisdom Teeth

Your OMFS surgeon will make an incision on the gums. He will then remove part of the bone surrounding the wisdom tooth and extract the tooth. Occasionally, he may need to cut the tooth in many pieces to safely remove it. The cut in the gums will be closed with dissolvable sutures.
- After surgery, you will need to follow the instructions provided by your surgeon (link)
Possible Complications
Like any other surgical procedure, removal of wisdom teeth has potential risks. Your OMFS surgeon will discuss these risks prior to your surgery, so that you can make an informed decision, weighing the potential benefits of having the procedure versus the risks. The most common complications are:
- Numbness or paraesthesia of the lip, chin and tongue
The wisdom tooth and its roots lies very close to two nerves; the inferior dental nerve that provides feeling to the half of the lip (on the same side) and the lingual nerve, that provides sensation and carries taste fibers for the anterior two thirds of half of the tongue (on the same side). When the wisdom tooth is extracted, these nerves may become bruised or injured. In the case of the inferior dental nerve, bruise can cause numbness or altered sensation (tingling, pain, “pins and needles”) in the lower lip, chin and the teeth of that side of the jaw. In the case of the lingual nerve, half of the tongue might be numb and there is also a risk of altered taste. It is important to mention that none of these nerves affects movement of the lip or the tongue.
If a nerve is injured, it goes through a phase called neuropraxia (temporary weakness) and it generally heals well afterwards. For most of the cases, complete resolution of the symptoms occurs within a couple of months, although some cases recover very slowly, and it might take up to 18 months to completely resolve. Very rarely, numbness or altered sensation can be permanent (about 1% of the cases). If numbness on the tongue persists for more than 2 months following a wisdom tooth extraction, your OMFS surgeon might explore the area and repair the lingual nerve using microsurgical techniques. However, this isn’t possible for the inferior dental nerve.
- Dry socket
This happens when the clot that normally forms in the healing process following a tooth extraction, doesn’t form or dissolves away. This leaves behind exposed bone, and is associated with constant, throbbing pain, that may last for several days. Smoking is the primary risk factor for the development of dry socket. You need to see your OMFS surgeon if this occurs, as the wound might need dressing
- Infection
- Bleeding
- Damage to a nearby tooth or fillings
- Oroantral communication
The roots of the upper wisdom teeth are very close to the sinus. Sometimes, following an upper wisdom tooth extraction, a hole might be cause to the floor of the sinus. Your OMFS surgeon will repair it if it happens, but occasionally sinus infection might occur.