Dental implants
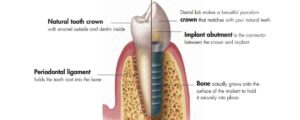
Dental implants are now a well-established technique for replacing missing teeth, and they are considered the gold standard for dental rehabilitation. They way they work is fairly simple: Your OMFS surgeon places a titanium screw into your jawbone (the “implant”) that acts as the root of the missing tooth. Your dentist then restores the implants with crowns, bridges or dentures, in a similar way to the way that roots support natural teeth.
The principle behind dental implants success is osseointegration.
Like many other great discoveries, this was also a matter of lack or fortune: In the 1950s, experiments were contacted fitting titanium chambers in the bones of rabbits. When an attempt was made to remove these chambers, it became obvious that this wasn’t possible, as the titanium has merged solidly with the bone. Branemark was then introduced the term osseointegration to describe the interaction of the titanium implant with the bone: After the implant is fitted, the bone surrounding it gradually grows up and attaches to the implant, holding it firmly in place.
A single dental implant can support one, or several, replacement teeth – so you don’t need to have one implant per replacement tooth. Implants can also be used to support a full or partial set of dentures. Your OMFS surgeon and your dentist will work together to plan as to how many implants you need, where they need to be placed and what type, shape, or size they need to be.
With appropriate care, your dental implants can last for as long as your natural teeth (or longer).
The process of getting dental implants
You need to be aware that the process of getting implants can take few appointments and up to several months to complete. This of course depends on each individual case, and your OMFS surgeon and your dentist will discuss the details with you.
In general, the process has 3 stages
- Placement of the dental implant into your jawbone by the OMFS Surgeon
- Osseointegration period (2-4 months). At the end of this period, a healing abutment is placed on the implant, to facilitate healing of the gums around the neck of the implant
- Construction and fitting of your new teeth onto your implants by your dentist.
The surgery

Placement of implants is a minor dentoalveolar procedure done under local anesthetic (link to the local anesthetic instructions). Prior to the procedure, your OMFS surgeon will take a full medical history, record your medications and discuss the details of the procedure with you. You will have some X-rays (OPG and maybe a cone beam CT), to assess the amount and quality of the bone. Occasionally, a surgical guide – splint will be made, to guide the positioning of the implants. Your OMFS surgeon will also explain the limitations of any realistic treatment with implants. They aren’t suitable for children and young people under the age of 18 because the underlying bones are still growing. There are some relative contraindications for having dental implants, and those are:
- Pregnancy: Although not impossible, it is advisable that pregnant women should wait until they have given birth before having their implants.
- Inadequate jawbone: If the bone of the jaw isn’t enough to accept implants, then other procedures should be considered prior to implants’ placement (link to bone grafting)
- Immunosuppression, diabetes and long term steroid use
- History of poor oral hygiene and severe periodontal disease
- Smoking, drug and alcohol abuse: These can lead to delayed healing and compromise osseointegration.
- Bisphosphonates
- Previous radiotherapy for H&N cancer: This is a field of scientific research and debate, however, it is generally accepted that for a patient who needs radiotherapy and implants, then it is better to have the implants placed prior to radiotherapy
Surgical steps

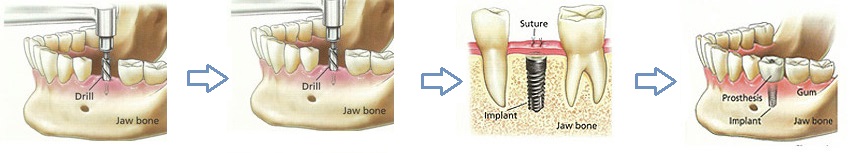
- Extraction of teeth (if not done already)
- Bone grafting if needed (link)
- Gum incision, bone exposure, hole drilling, implant placement
Once the implant is placed, the abutment that will hold the false tooth in place will be fitted to the implant. This can be done in one of two ways:
- Single stage or immediate: the implant and the abutment are fitted at the same time.
- Two stages: the implant is placed and time is allowed for it to heal and achieve osseointegration. The abutment is then placed in a second minor procedure
Once the implants are placed and osseointegrated, your dentist will proceed to attach the replacement teeth to the implants. Your dentist will discuss the best option for you in your particular circumstances. You may have a temporary denture fitted until all of the work is completed.
Success rate
Success depends upon a number of factors, including:
- The skill of the surgeon
- Whether you smoke or have diabetes
- Your oral hygiene
- The position of the implants
- Your general health.
You should expect a 95% success rate, which is even higher with careful case selection
Complications of implant surgery
Like any other surgical procedure, placement of implants has potential risks. Your OMFS surgeon will discuss these risks prior to your surgery, so that you can make an informed decision, weighing the potential benefits of having the procedure versus the risks. The most common complications are:
- Nerve damage: The inferior dental nerve that provides feeling to the half of the lip travels within the mandible underneath the roots of the teeth. If the implant placement isn’t planned properly, the drill or the implant itself might injure this nerve. This will result in numbness or altered sensation (tingling, pain, “pins and needles”) in the lower lip. This can be temporary or permanent, depending on the extent of the damage. Careful planning with X-rays and cone beam CT reduces the risk of nerve damage.
- Implant failure: The implant won’t integrate with the jawbone, and will become loose. In that case you may need to have another implant, or consider other options for dental rehabilitation, depending on the cause of the failure.
- Perforation of sinus or nasal floor
- Damage to adjacent teeth
- Fracture of the mandible (in cases of weak jaws, i.e. severe osteoporosis)
- Infection
Special considerations
Zygomatic implants
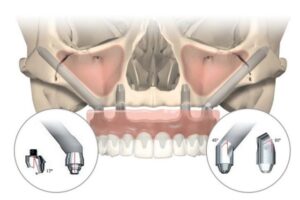
Patients with severely resorbed maxillary bone and maxillary atrophy may benefit from the placement of zygomatic implants. These use the same principles of osseointegration, but they are larger and longer, as they are placed into the zygoma bone. They emerge at the posterior maxilla at an angle; they therefore require specially designed angulated abutments. They offer high primary stability, they can be loaded and function immediately, and offer significant surgical flexibility.
They are particularly useful for patients that will otherwise require large volumes of bone grafting. The procedure to insert zygomatic implants has less morbidity and is less invasive than bone grafting. They can also be used following cancer resection of the maxilla, when bony reconstruction isn’t feasible.
The success rate in experienced hands is over 95%. The procedure can be done under local anaesthesia, using an intraoral incision to access the maxillary buttress and the zygoma bone.