Patient-Specific Three-Dimensional Planning for Head and Neck Reconstruction: Paradigm Shift and Refuted Myths
Patient-specific planning and three-dimensional printing have revolutionized head and neck reconstruction.1 Tumor resection/flap harvesting are guided by laboratory-made guides using the patient’s scan data. This leads to the downfall of many surgical myths.
Myth 1: Extensive mandibular resections are common. A fibula flap has been the gold standard, because of bone length. However, the fibula is of low height, which makes placement/rehabilitation of dental implants challenging. Cosmesis, contour/profile, and the reliability/pliability/flexibility of the skin paddle are questioned.
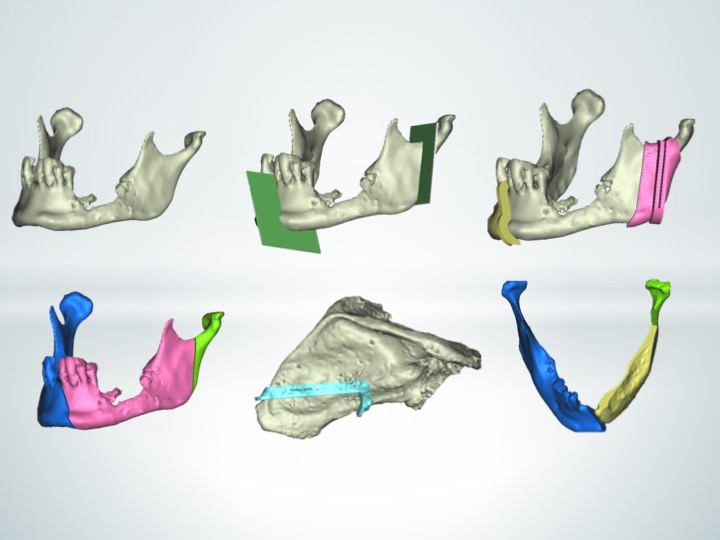
Using patient-specific planning/three-dimensional printing, we realized that chimeric scapula flaps work in these defects. The average angle-to-angle mandible length is 10 to 12 cm,2 equal to the length of the available scapula bone. [See Figure, Supplemental Digital Content 1, which shows angle-to-angle mandibular reconstruction with a chimeric scapula free flap based on the circumflex scapular artery and the angular branch. The soft-tissue component was based on the thoracodorsal artery (not shown here), https://links.lww.com/PRS/E869. See Figure, Supplemental Digital Content 2, which shows angle-to-angle mandibular reconstruction with a chimeric scapula free flap based on the circumflex scapular artery and the angular branch. The soft-tissue component was based on the thoracodorsal artery (not shown here). Dental rehabilitation was achieved with guided/planned osseointegrated dental implants, https://links.lww.com/PRS/E870.] This allows harvesting a reliable/large/pliable skin paddle based on the thoracodorsal vessels.
Myth 2: A deep circumflex iliac artery (DCIA) flap for maxillary reconstruction is feared because of the short pedicle. The distance between the maxillary tuberosity and the antegonial notch is 5 cm.3 Add 2 cm and one reaches the external carotid. The average DCIA pedicle length is 5.5 to 7 cm. What is the issue then? Using patient-specific planning/three-dimensional printing, we realized how crucial is the inset/positioning of this flap. One should design the shape/position so that the pedicle emerges at the lowest/most posterior part (tuberosity) and harvest the flap distal to the anterior superior iliac spine. (See Figure, Supplemental Digital Content 3, which shows reconstruction of a class IV maxillectomy defect with a patient-specific planning/three-dimensional printing DCIA free flap, https://links.lww.com/PRS/E871. See Figure, Supplemental Digital Content 4, which shows reconstruction of a class II maxillectomy defect with a patient-specific planning/three-dimensional printing DCIA free flap. The possibility of a zygomatic implant perforator flap was explored but excluded, as the patient was dentate with a high contralateral maxillary alveolus, https://links.lww.com/PRS/E872.)
Myth 3: One of the arguments against scapula flaps in the head and neck is the difficulty for dental implant rehabilitation. Using patient-specific planning/three-dimensional printing reveals that this is not true. With careful planning, we insert implants in the majority of patients. (See Figure, Supplemental Digital Content 5, which shows reconstruction of a hemimandibulectomy defect with a scapula tip flap based on the angular branch. Note the combined mandible/flap implant planning and guide, https://links.lww.com/PRS/E873.) Using the angular branch allows harvesting the thicker scapula part, which can host virtually any implant size. [See Table, Supplemental Digital Content 6, which shows the osseointegrated implants success rate in relation to free flaps. PSP, patient-specific planning, https://links.lww.com/PRS/E874.]
Myth 4: Minimizing morbidity for elderly patients is challenging. If fit for free flap surgery, one should explore the option because of its higher quality-to-morbidity ratio. A fibula flap is low on the list (peripheral vascular disease, donor-site healing). A composite radial seems tempting (double team operating); however, the bone quality is limited and there is a risk of radius fracture. When possible, we favor scapula flaps. (See Figure, Supplemental Digital Content 7, which shows a successful reconstruction of a hemimandibulectomy defect with a scapula tip flap based on the angular branch in an elderly patient with peripheral vascular disease and diabetes, https://links.lww.com/PRS/E875.) These are reliable and offer abundant bone/soft tissue.
Myth 5: The personalized patient-specific planning of soft-tissue reconstruction flaps4 shows that patient-specific planning/three-dimensional printing is not limited to bone. In fact, the potential cosmetic/functional benefits might be greater for soft-tissue head and neck reconstruction. Patient-specific planning/three-dimensional printing allows the transformation of a three-dimensional defect into a two-dimensional flap outline/perimeter, with volumetric assessment.
Myth 6: Our growing patient-specific planning/three-dimensional printing experience has shifted our flap choices/selection. We now use scapula, DCIA, and fibula flaps in a ratio of 50:35:15 percent, in contrast to other units. We believe that this is because of training/availability of skills/recourses. Similarly, the concept that the fibula skin paddle can solely fail is poorly proven; one would argue that fibula is less reliable than other bony flaps.5 “Don’t treat everything as a nail, because you have a hammer.”
Myth 7: Patient-specific planning/three-dimensional printing is the standard of care in many centers. However, it is not uncommon to see press releases about “novel three-dimensional leg bone–jaw reconstruction.” In 2020, advertising patient-specific planning/three-dimensional printing in such a way seems misleading. Nowadays, surgeons should come together and share knowledge/experience in the correct forums. Let us encourage scientific collaboration instead of self-promotion.
Patient-specific planning/three-dimensional printing has revolutionized head and neck reconstruction. Many myths have been refuted, and it is in our (surgeons/researchers) hands to use it/develop it.